…𝒉𝒐𝒘𝒆𝒗𝒆𝒓, 𝑯𝑷𝑽 𝒗𝒂𝒄𝒄𝒊𝒏𝒂𝒕𝒊𝒐𝒏 𝒄𝒂𝒏 𝒑𝒓𝒆𝒗𝒆𝒏𝒕 𝑯𝑷𝑽 𝒊𝒏𝒇𝒆𝒄𝒕𝒊𝒐𝒏 𝒂𝒏𝒅 𝒓𝒆𝒅𝒖𝒄𝒆 𝒕𝒉𝒆 𝒊𝒏𝒄𝒊𝒅𝒆𝒏𝒄𝒆 𝒐𝒇 𝒄𝒆𝒓𝒗𝒊𝒄𝒂𝒍 𝒄𝒂𝒏𝒄𝒆𝒓, 𝒘𝒉𝒊𝒍𝒆 𝑯𝑷𝑽 𝒕𝒆𝒔𝒕𝒊𝒏𝒈 𝒄𝒂𝒏 𝒅𝒆𝒕𝒆𝒄𝒕 𝑯𝑷𝑽 𝒊𝒏𝒇𝒆𝒄𝒕𝒊𝒐𝒏 𝒂𝒕 𝒂𝒏 𝒆𝒂𝒓𝒍𝒚 𝒔𝒕𝒂𝒈𝒆, 𝒇𝒐𝒓 𝒕𝒊𝒎𝒆𝒍𝒚 𝒕𝒓𝒆𝒂𝒕𝒎𝒆𝒏𝒕 𝒂𝒏𝒅 𝒑𝒓𝒆𝒗𝒆𝒏𝒕𝒊𝒏𝒈 𝒄𝒂𝒏𝒄𝒆𝒓
Phurpa Wangmo
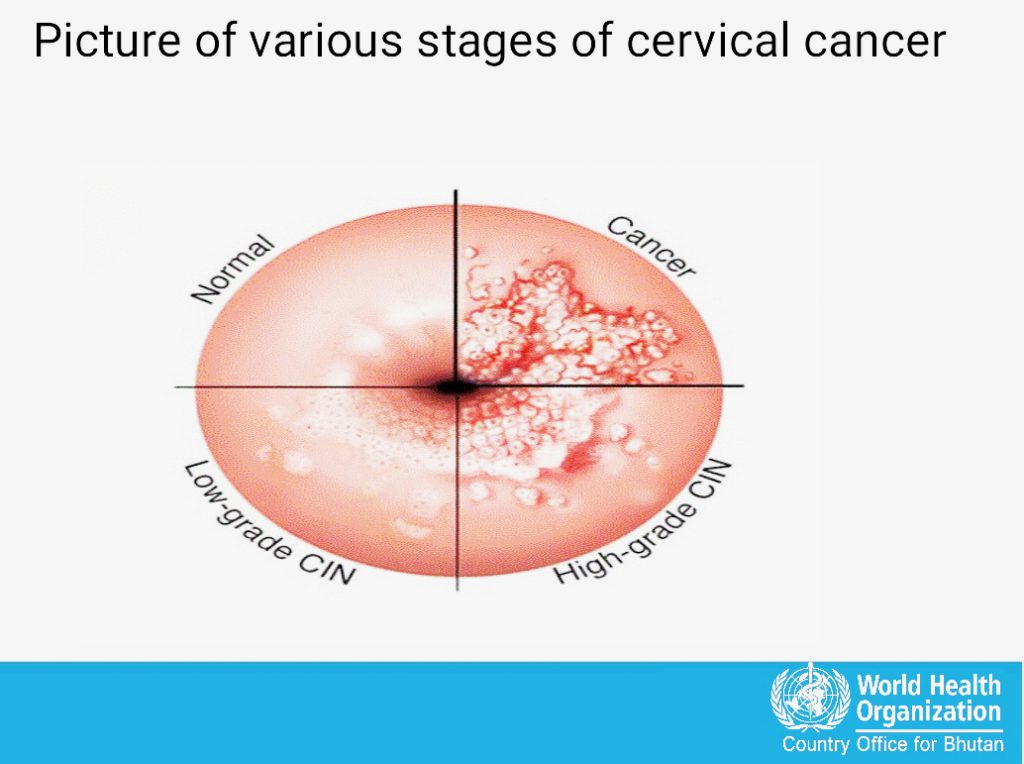
Cervical cancer is the most prevalent cancer among women in Bhutan. It has a high mortality rate and is a major public health concern in the country. More than 300 cases of cervical cancer were reported across the country in between 2014 and 2018, out of which 30% were diagnosed in advanced stages. The estimated age incidence and mortality for cervical cancer is 20.5 and 4.7 per 100,000 women respectively and to further complicate the matter, cervical cancer is detected at a stage when women are most socially and economically productive
The eligible women for HPV testing are between 30-65 Years old in Bhutan. HPV (human papillomavirus) infections are very common, especially in young women who are sexually active. HPV is a virus that spreads through sexual contact. It causes cervical cancer and other cancers. The HPV vaccine can protect you from HPV and the cancers it causes.
However, most HPV infections are cleared by the immune system within a year or two without causing any long-term health problems. Thus, all sexually active and married women under 30 years are not enrolled in the current screening program.
However, there are some women who are reluctant to come forward for HPV testing since they are shy and some think it is only for married women.
Tashi Tshomo, Program Officer, Department of Public Health under Ministry of Health(MoH) said, “Although there might be some women who are not coming for screening, we are ensuring that all eligible women avail the screening service through intensified advocacy and awareness.
Tashi also said, “They are engaging Civil Society Organisations (CSO) and local government in the advocacy program to ensure ownership of the program and moreover, they are also encouraging women who are shy to undergo self-sampling of HPV test”.
“The risk of developing cervical cancer increases with age, with the highest incidence rates observed in women over the age of 30.The age range of 30-65 years old is recommended for HPV testing in women because this is the age range where HPV infections are most likely to persist and lead to cancer, and the benefits of screening with HPV testing outweigh the risks”, added Tashi Tshomo.
HPV vaccination can prevent HPV infection and thus reduce the incidence of cervical cancer, while HPV testing can detect HPV infection at an early stage, allowing for timely treatment and prevention of cervical cancer.
Thus, in the post-vaccination period, Pap smear screening will be less useful as there will be decrease in the positive predictive value of cervical screening with cytology. New revised policies considering introduction of HPV detection based screening was considered for improving efficiency of screening program in the post-vaccination era under the Health Flagship Program.
Introducing HPV testing can provide an opportunity to link screening with HPV vaccination programs which was introduced in Bhutan in 2010, as both interventions are essential for the prevention of cervical cancer.
Cervical cancer is the fourth most common cancer among women globally and in 2019, more than 70 countries supported the decision of WHO secretariat to develop a Global Strategy towards the elimination of cervical cancer.
Conventional cytology (Pap smear) has been the primary screening method for cervical cancer for many years, but it has several limitations. Pap smear tests are subjective and can produce false negatives and false positives. Additionally,
Pap smear tests require trained laboratory staff, and they are relatively expensive and time-consuming.
In contrast, HPV testing is a more sensitive and objective method for detecting cervical cancer. HPV testing detects the presence of high-risk HPV types that are associated with cervical cancer. HPV testing is also more cost-effective in the long run compared to Pap smear tests, as it requires fewer tests and reduces the number of unnecessary follow-up visits.
Dr. Lobzang Dorji, National Professional Officer of World Health organization (WHO) said, “The risk factors for cervical cancer includes early age of sexual debut and early age at first child birth, multiple sexual partners , multiple child birth, smoking , a week immune system and also not getting vaccination and screening is at the biggest risk”.
He also said that in 2020, WHO Global strategy was developed to accelerate the elimination of cervical cancer as a public health problem.
In the journey towards elimination of cervical cancer, Bhutan was also the first country in the Southeast Asia region to introduce HPV vaccination for adolescent boys which has been integrated into the routine immunization program since 2020. Each year, more than 95% of both the adolescent girls and boys are vaccinated against HPV.
Ministry of Health has screened more than 85 percent of all the eligible women under the health flagship program after the introduction of Human Papillomavirus (HPV) testing replacing the conventional pap smear.
 BHUTAN TODAY The New Perspective
BHUTAN TODAY The New Perspective
